Since the dawn of healthcare education, one patient demographic has demanded special attention. Falling into the literal category of "special populations," they're cordoned off and talked about with an almost bogeyman-like reverence. This population?

None other than the terrifying child.
Why are we all terrified of children? Apart from the obvious—higher stakes, lower opportunity, stressed parents...I think a great deal of this anxiety and fear we all have might be due to the way we're taught.
The Mantra We Teach: "They Are NOT Little Adults"
Every nursing class. Every EMT textbook. Every CE lecture on pediatrics. They all hammer the same mantra: "Children are NOT little adults."
The intended message is solid: don't blindly apply adult normal values to kids. Don't dose medications like you're treating a miniature human. Don't assume a kid's airway is just a scaled-down adult airway. All valid points.
Where Our Teaching Backfires: Fear-Based Lessons
But here's how that message often lands: kids are essentially a different species. We're often told to forget everything we know about physiology with relation to adults as we move into a pediatrics focused class. We immediately begin learning about incredibly nuanced and complex congenital diseases. We have multiple different methods for remembering their bizarre vital signs thrown at us with brand new "normals" that we need to know. These lessons always left me feeling as if kids worked on some mysterious different physiology, that their vital signs and assessments were enigmatic, and that above all → I should be afraid of kids.
"Children are not little adults" is true, but it's often taught in a way that causes fear instead of understanding. The real message should be: same physiology, smaller size, narrower margins.
The Reality: Same Science, Different Proportions
Here's the truth that gets buried under all the anxiety: pediatric patients follow the same core physiological rules as adults. The parameters are different. The margins are tighter. But the underlying science? It's the same.
Let's break this down:
Ventilation & Oxygenation
Same V/Q concepts. Same gas exchange principles. Same relationship between minute ventilation, tidal volume, and respiratory rate. Kids just have higher metabolic demands, so they run at faster respiratory rates to keep up. A 6 month old's oxygen demand per kg is roughly double that of an adult (1). But the mechanics? It's the same.
Shock & Perfusion
Same compensation mechanisms in response to shock. Tachycardia, vasoconstriction, catecholamine surges. All work the same way as an adult at base with some special caveats. As we've all probably been taught a million times, kids compensate until they don't. Their compensation mechanisms work so well that they can just floor it til the wheels fall off. So we do need to pay attention to how long they've been compensating. But the physiology is all the same!
Pharmacology
Same receptors. Same drug classes. Epinephrine still works on alpha and beta receptors. Ketamine still dissociates. Fentanyl is still an analgesic. We use weight-based dosing because absolute doses need to match body size, and we consider developmental pharmacokinetics, but the fundamental pharmacology hasn't changed just because the patient is shorter.
Think of it this way: it's the same physiology, running faster, with tighter margins
Where "Not Little Adults" Reigns True
We aren't taught this for no reason though. So there really are some genuine peds-specific differences that we need to know.
Anatomy + Airway
Kids have big-ass heads, bigger tongues relative to their oral cavity, a floppier epiglottis, and narrower airways. The narrowest point in a kid's airway is at the cricoid ring, not the vocal cords like in adults. These differences matter when you're managing an airway. They don't mean kids breathe through a different mechanism than adults.

Circulating Volume
A kid's total blood volume is actually higher per kilogram than an adult's (~80 mL/kg vs. ~70 mL/kg), but their absolute volume is much smaller. A 10-kg toddler has about 800 mL of blood (2). That means what looks like "a little bleeding" to you might represent a significant percentage of their total volume. Same physiology, smaller reservoir.
Arrest Etiology
Adults arrest from cardiac causes. They throw clots, they have ischemic events, they go into lethal arrhythmias. Children though? We know this, we've been beaten over the head with this forever—kids arrest from hypoxia and shock. That's going to be respiratory failure and most likely sepsis or dehydration. Just like we have our H's and T's with adult arrests, kids are the same: we're just going to have a stronger index of suspicion towards the aforementioned.
The mantra is valuable when it pushes you to respect and adapt. It backfires when it makes you panic and freeze. Know the differences, but don't let them convince you that everything you know about medicine suddenly doesn't apply.
Where the Mantra Backfires: Fear-Based Teaching
Let's talk about how we actually teach pediatrics in EMS, nursing, and critical care education.
Seriously: how many of your pediatric lectures felt like campfire horror stories?
"Kids crash fast. One minute they're fine, the next they're coding."
"You mess up the dose and you'll kill them."
"Pediatric arrests have terrible outcomes."
All technically true statements that only serve to scare and intimidate. They're all absolutely useless for building clinical competence.
It also doesn't help when the lecturer is just as intimidating as the words they're saying. The majority of the time, this content is taught by seasoned pediatric ICU nurses. Which is phenomenal; however, they have this habit of being really scary for some reason... (JJC nursing will understand).
Then there's the memorization problem. Here's a chart for normal heart rates, vaccinations you need to memorize, blood pressure formulas, weight estimation formulas, formulas for ET tube sizes and on and on and on. We're inundated with infographics and tips all focused on this one population. Which in an ideal world is great! But it's total information overload and causes more fear and hesitancy. I personally think that using a unified and comprehensive reference/calculator for all things pediatrics is super helpful and alleviates a lot of the panic as we try to remember where xyz reference was.
Shout out the holy grail of peds calculators:
https://calculator.nets.org.au/ClinCalcMenu.php
The consequences of fear-based teaching are real and visible:
- Providers freeze on pediatric calls, overthinking simple problems
- Providers abandon the adult pathophysiology they already understand
- Providers avoid pediatric training and simulation because it's anxiety-inducing
I've watched phenomenal paramedics who I've seen manage intense traumas absolutely freeze at the sight of a 2 yo with difficulty breathing. That's not a knowledge problem. That's a confidence problem, created over years of being told that kids are scary and fragile.
Soooo what do we do then?
I don't know im just some guy yapping on his website. But here's some palces we can start immediately: our tools and calculators!
Length-Based Tapes
Broselow, Handtevy, whatever your system uses. These aren't cheating. They're evidence-based tools that remove cognitive load so you can focus on the patient. Get them out and look at them... Seriously, I know people who are afraid to even look at these things because they're stress inducing. You do not want to be pulling this fucker out without having looked at it in years. You'll thank me.
The Pediatric Assessment Triangle
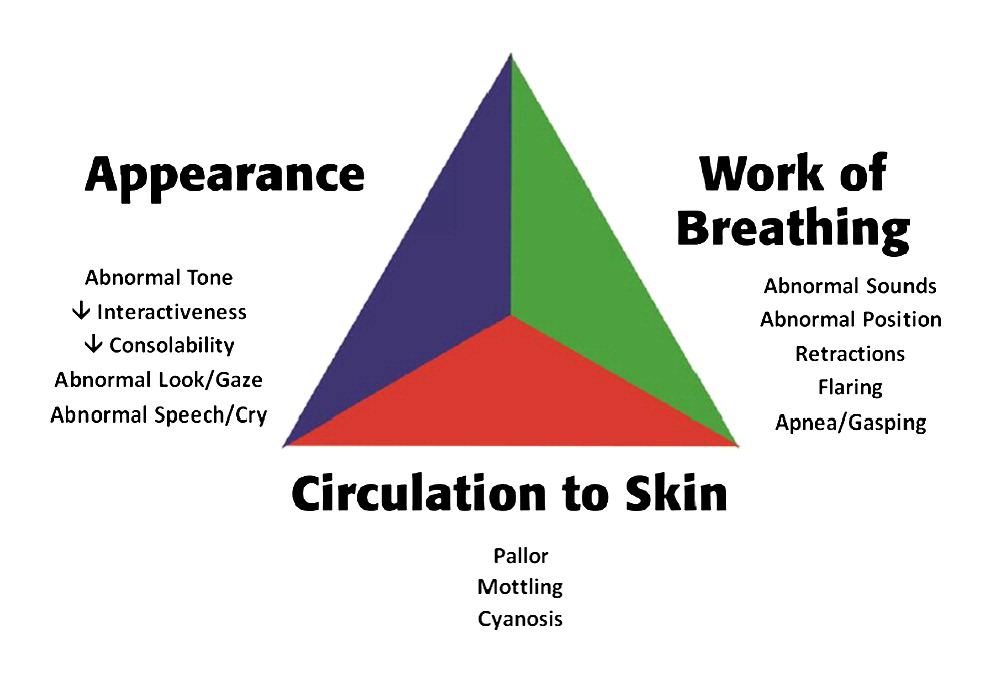
Appearance, Work of Breathing, Circulation to Skin. This takes literally three seconds and tells you if the kid is sick or not sick before you even touch them. It's the same "doorway assessment" you do on adults, just formalized.
Get used to doing this on EVERY kid. We struggle to get accurate NIBP readings on so many of these sick kids and the best indicator of poor perfusion/shock is the assessment. Cap refill is a great surrogate for BP.
PALS Algorithms
Structured approaches that guide your thinking. They exist because even experts benefit from cognitive aids in high-stress situations.
The point is: these tools let you use the medicine you already know. You understand shock. You understand respiratory failure. You understand the importance of early intervention. The tools just help you scale that knowledge to a smaller patient.
Culture Change: How We Talk About Pediatric Calls
If you're an educator, preceptor, or experienced clinician, this part is for you.
Stop using pediatric cases as campfire horror stories. Yes, they can be intense. Yes, outcomes can be devastating. But leading with fear creates individuals who avoid, freeze, or panic.
The Bottom Line
Kids are not monsters. They're not a completely different species that defies everything you learned in your adult training.
"Children are not little adults" is half true, but it's often taught in a way that causes fear instead of understanding. The real message should be: same physiology, smaller size, narrower margins.
You already know how shock works. You already know how respiratory failure progresses. You already understand the importance of early recognition and intervention. That knowledge doesn't disappear just because your patient is small, fat, and cute.
Practical Clinical Pearls
Everything you know about shock, respiratory failure, and resuscitation still applies. You're not learning a new specialty >>> you're adapting the one you already have.
A normal blood pressure doesn't mean the kid is fine. Watch mental status, work of breathing, cap refill, and pulse quality. By the time the BP drops, you're already behind.
A heart rate of 150 in a screaming toddler is meaningless. A heart rate of 150 in a quiet, pale, limp toddler is terrifying. Context matters more than the number itself.
Fix oxygenation, ventilation, perfusion, and glucose before you chase zebras. The vast majority of pediatric emergencies are bread-and-butter problems: respiratory distress, dehydration, seizures. Not every kid will have tetralogy of fallot; no matter how many times you had to learn about it.
(1) National Research Council, & Institute of Medicine. (2004). Children's health, the nation's wealth: Assessing and improving child health. The National Academies Press. https://doi.org/10.17226/10886
(2) The Royal Children's Hospital Melbourne. Circulation management. Trauma Service Manual. Retrieved from https://www.rch.org.au/trauma-service/manual/circulation-management/

